The flight team arrived and got him ready to travel. I couldn’t go with him in the helicopter. I’ve never felt so scared to leave my baby. I felt nauseous. He would arrive within 30 minutes flying but it would take us two hours to drive. We knew that if we were going to Duke, we would be staying there for at least a few days. We went home and grabbed a few things before making the longest drive up to the hospital.
Once he arrived at Duke, Thomas was placed in the Pediatric Intensive Care Unit (PICU). Thomas continued to receive treatments to open his airways and move secretions out of his lungs. He was on BiPAP when we arrived and later that day he was intubated. Because we didn’t know if he had a virus or not, Thomas had to be isolated. We had to wear a mask, a gown, and rubber gloves when we were close to him.
On March 2nd, we were approved to stay at the Ronald McDonald house of Durham, a home away from home for 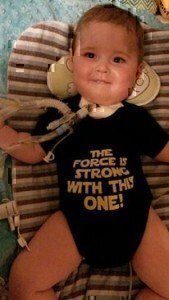 families who have critically ill children. The next day Hanna was able to join us at the house.
families who have critically ill children. The next day Hanna was able to join us at the house.
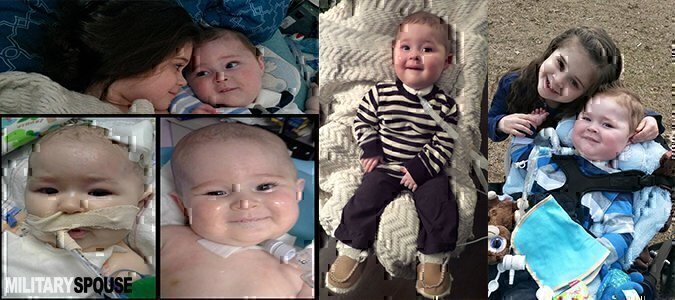
On March 7th, after 6 days of helplessly watching my son be poked and hooked up to machines, I was able to hold him. It was an amazing feeling. I have since held him every day. Each day feels a little better than the day before but not as good as I knew the next day would feel.
The blood work came back on March 10th confirming his diagnosis of SMA – type 1. It was like the knife that stabbed me in the back was twisted. The blood work made it final.
On March 13th, he had surgery for g-tube and Nissen fundoplication or stomach wrap. SMA Type 1 children usually lose the ability to chew and swallow food and water safely. This can happen at different times for each child. Continuing to take in food and water by mouth can result in a high risk for aspirating and developing respiratory problems such as aspiration pneumonia. To prevent these complications, tube feeding is used to ensure he will get enough calories to grow and enough fluids to remain hydrated.
 On April 7th, he was ex-intubated to BiPAP. He was able to be to maintain adequate support for about 6 hours before his blood gas was too high and he began to run out of energy. This resulted in taking a few steps backwards in having to be re-intubated.
On April 7th, he was ex-intubated to BiPAP. He was able to be to maintain adequate support for about 6 hours before his blood gas was too high and he began to run out of energy. This resulted in taking a few steps backwards in having to be re-intubated.
With few options left, we decided to schedule a tracheostomy surgery to provide stable airway for him. The surgery took place on April 10th.
On May 12th, after 73 days of being in the hospital, we were discharged to go home. Going home was exactly what we wanted but nothing like what we expected. We brought our baby home with two holes in his body and tubes coming from each, one to eat and one to breathe. The tubes were connected to machines that were always running. Accompanying us in our home were nurses that helped care for Thomas while we slept because of his extensive care requirements.