Article by Heidi Smith Luedtke, Air Force Spouse
I was thrilled when I got pregnant just six weeks before my spouse was scheduled to
deploy to Iraq. The timing was perfect-he’d be gone for the second trimester and home before my due date.Military family planning isn’t always so easy. And even when the stars seem to be aligned in your favor, it doesn’t always work out the way you expect it will.
Everything changed when that deployment led to another, much longer one. I chose to move closer to family, and that meant packing up by myself and switching
obstetricians in my eighth month. I worried about my health and wondered how the baby
would bond with my spouse, who wouldn’t come home until our son was 15 months old.

Even in the best circumstances, pregnancy is an emotional roller coaster. “Powerful feelings of vulnerability can creep in the second we start considering getting pregnant,” says Brene
Brown, Ph.D., author of “Daring Greatly: How the Courage to Be Vulnerable Transforms the Way We Live, Love, Parent, and Lead.” You may wonder if you can get pregnant and stay pregnant, especially if you’ve had previous miscarriages. You may feel an enormous sense of responsibility for your unborn child and want to do everything right. “We fear the inability to protect people we love,” Brown says.
“It’s very common for women to feel powerless, overwhelmed and confused during pregnancy,” says nurse practitioner Camilla Bicknell, former Navy nurse captain and co-author of “The Pregnancy Power Workbook.”
New worries crop up at each stage. Early on, surging hormones, morning sickness and fatigue may keep you from feeling your best. At the same time you wade into a flood of medical information; it’s hard to make sense of it all.
MID-PREGNANCY IMPROVEMENT
During the second trimester, you may feel better physically. But planning for baby’s arrival brings more worries. PCS moves and deployments can increase your stress level and make you feel especially out of control, Bicknell says. Being far away from family also increases
the sense of vulnerability. As your due date approaches, fears about labor pain and delivery
complications may keep you up at night. You may think about worstcase scenarios and draft a detailed birth plan, hoping to regain control. Deep down you may still feel afraid.
“Pregnancy and motherhood are two of the most vulnerable experiences in the whole human experience,” Brown says.
RECLAIM CALM
Although you can’t control every aspect of pregnancy, you can increase your sense of personal empowerment. Here’s what the experts advise:
Study Up: Information about pregnancy is everywhere and it can make you feel anxious
about your diet, and medical risks. “Be prepared for your prenatal appointments with a list of questions,” encourages Bicknell. Your provider might only have a couple of minutes to chat and she may assume you don’t have concerns if you don’t ask questions.
Show your list to the provider so you don’t forget to speak up when you’re feeling exposed.
Tailor your questions to your personal medical history and your stage
of pregnancy so you get actionable information. You will feel most empowered if you focus
on what you can do this week and this month to improve your health and give your baby the best possible prenatal environment.
Financial issues can also cause a great deal of stress. “Meet and make contact with the MTF-based Tricare rep,” says Tricare perinatal and special needs nurse consultant
Theresa Hart, RNC, MS. They should be able to answer questions about your insurance coverage and any out-of-pocket expenses.
If you have other insurance, find out what’s covered so you aren’t surprised later.
Build a Team You Trust: “An OB team approach works well for many women,” says Bicknell. And you’re the star player on the team. Your roster should include your spouse, a family member or friend (especially if your spouse is not available), your OB provider, your regular doctor, and other staff members at the clinic.

“If you still feel like you and your provider are not on the same page, ask to switch to another provider,” Bicknell advises. It may seem risky to change from a doctor you know to one you haven’t yet met. Do it anyway. You need a provider who listens to you and allows you to be actively involved in your health care.
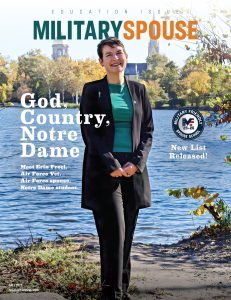
Cover Photo: Elizabeth Boggs
Photo Credits in Order: Erin Whitehead, Raina Sky, Ginny Haupert
Lean Into It: “Vulnerability is difficult,” Brown acknowledges, but it’s also “the
birthplace of love, trust, empathy and joy.” When you feel the simultaneous rush of excitement and fear, move toward it rather than running away. Let yourself feel the entire range of emotions – even the scary ones. “It takes courage to be real,” Brown says.
As a military spouse, you’ve probably had lots of experience with uncertainty. Acknowledge
you won’t be able to make everything happen according to your personal pregnancy plan
and do your best to take care of your health and well-being. One thing is for sure: babies have plans of their own.